Cephalic Duodeno Pancreatectomy
- Right subcostal incision
- 3 anastomoses: pancreaticosplenic gastrostomy, duodeno-jejunostomy and hepatico-jejunostomy
- Admission the day before surgery
- No bowel preparation required
- Operating time 3.5 hours
- Nasogastric tube for 5 days
- Bilateral drainage
- Length of hospital stay 15 days on average
Pancreatic cancer tends to occur quite late in life, around 70 years old.
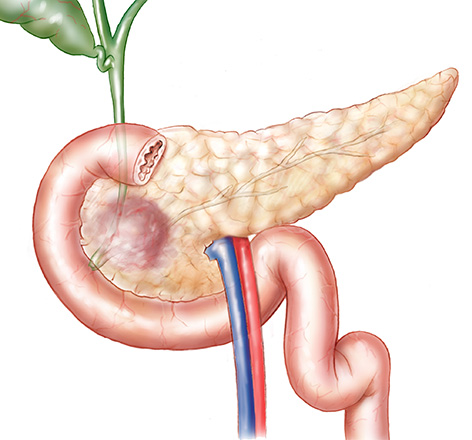
The pancreas is both an exocrine (secreting digestive enzymes) and endocrine (secreting insulin and other hormones) gland located behind the stomach and contiguous to the duode-num and the main bile duct.
Some tumours that are initially benign may become cancerous, such as IPMN (Intraduc-tal Papillary Mucinous Neoplasms) which are diagnosed at a stage of cancer in about 30% of cases.
The association of the 3 following symptoms should make this diagnosis a priority in people over 60 years: jaundice, gastric pain and weight loss.
Additional tests to be carried out in priority are :
- Thoracoabdominopelvic CT scan
- Endoscopic ultrasound, performed by a specialised gastroenterologist. This examination is to be made when there is doubt about the benign or malignant nature of the tumour, or if the tumour cannot be seen on the scan.
Once the diagnosis is made, the various specialists (surgeons, oncologists, radiologists, gastroenterologists) will evaluate whether the tumour can easily be removed surgically. The operation is possible in about 25% of cases. Its purpose is to remove the tumour in its entirety.
When the tumour is localised in the head of the pancreas, the operation offered by the surgeon is the CDP (Cephalic DuodenoPancreatectomy). It consists in removing the head of the pancreas, the duodenum and the main bile duct. It is then necessary to reconstruct the cycle of digestion by performing 3 anastomoses.
The 3 main complications following this operation are :
- gastric emptying disorders
- pancreatic fistulas
- hemorrhages.
When the tumour is large (> 3cm), the relevance of preoperative chemotherapy is discus-sed with oncologists to evaluate the sensitivity of the tumour to chemotherapy and to facilitate complete resection of the tumour by making it regress in size.
In case of severe jaundice (pruritus and impaired renal function), it is necessary to put a prosthesis in the main bile duct during gastroscopic fibroscopy in order to “de-jaundicise” the patient before starting chemotherapy and perform the surgery.